How can we be better prepared for the next pandemic? This question will be the focus of WUR’s Dies Natalis (Founders Day) on 9 March. Guest speaker Henk Bekedam, who worked for the WHO for nearly 24 years, will offer an analysis. ‘Covid-19 exposes all the weaknesses in the healthcare system.’
‘I haven’t got involved in discussions about whether the schools should open or stay closed, or whether the curfew is a good idea,’ says Henk Bekedam. ‘I look at the coronavirus epidemic at a more systemic level. In my opinion, Covid-19 exposes the weaknesses of the healthcare system. We can and must learn from that.’
Henk Bekedam worked for the World Health Organization (WHO) for nearly 24 years. As WHO Representative, it was his job to advise on the SARS epidemic in China and the coronavirus crisis in India. He returned to the Netherlands last summer in the middle of the pandemic. He has since been appointed chair of the expert group that will advise the ministries of Health and Agriculture on how the Dutch healthcare system can be better geared up for coping with zoonoses. Wim van de Poel of WUR is in the expert group too.
‘The Netherlands has an excellent healthcare system when it comes to hospitals and GPs,’ says Bekedam. Market forces have made the system very efficient as well, but that also means it lacks the buffer with extra beds and staff that you need to cope with the initial impact of a pandemic. Bekedam also saw that the municipal health services (GGDs), whose budgets have been repeatedly cut over many years, lack the capacity to cope with the workload and additional tasks that fall to them during a pandemic. These include testing, contact tracing and vaccination campaigns.
‘The Netherlands spends a lot of money on healthcare, about 100 billion euros a year, but very little on prevention and safety – only about 200 million euros. The market doesn’t work on prevention and safety; the government must invest more in that itself.’
What can Wageningen contribute?
‘For prevention, I see an important role for Wageningen in terms of zoonoses, the viruses that can jump from animals to humans. Intensive livestock farming creates certain risks for the emergence and transmission of such diseases.
‘We must do more research on the effects of urbanization and deforestation, which bring wild animals in contact with humans more’
You need to do research on that, and on the impact of climate change, through which diseases can be spread more easily by mosquitoes. The Netherlands has a good system for surveillance of animal diseases. The development of avian flu, for instance, is monitored well and proactively, but there is no compulsory reporting on swine flu. Pigs generally don’t get sick from the flu, but pigs are genetically close to humans and some influenza viruses are easily transmitted from pigs to humans. So it is best to tackle the disease among the animals, which in this case means developing a flu vaccine for pigs.
‘We should also do more research on the effects on disease development of urbanization and deforestation, which bring wild animals in contact with humans more. Of course we need strict controls on the wet markets where live wild animals are sold. I read that the trade in wildlife has grown five times bigger over the past 10 years. In that case you can be sure that trade is going through Schiphol airport and the port of Rotterdam too. We need to identify and curtail those risks.’
Are there other preventive measures we can take?
‘I’m thinking of antibiotics as well. The misuse of antibiotics leads to resistant bacteria in the healthcare system. The use of antibiotics in livestock farming in the Netherlands has gone down by 70 per cent in the past 10 years without any economic damage to the sector. A nice example of Dutch preventive policy, but there is still a challenge there, because antibiotic use is still too high.’
Have we learned things from Covid-19?
‘Yes, this pandemic has exposed all the weaknesses of the system, both in the Netherlands and in the rest of the world. One of the challenges is that the virus also spreads via people who are asymptomatic. On the other hand, the lessons we are now learning from Covid-19 are similar to the lessons from other outbreaks. During the SARS epidemic of 2003, we learned that you must act fast when a new disease appears, and that preventing illness with testing and contact tracing is a very important part of combatting it. The countries in Asia that were affected by that epidemic, such as China, Taiwan, Thailand and South Korea, invested in labs and a better early warning and information system. That has paid off now with Covid-19. These countries identified the disease in time, took action fast, and therefore prevented a large-scale outbreak.’
What is the weakest link, do you think?
‘The pandemic shows that countries need to invest more in prevention and safety, including early warning systems. At the same time, we need a global approach to this global threat, and we should help the weaker countries. In the end we are only as strong as the weakest link.’
Dies natalis: Pandemic Prevention, Prediction and Preparedness. A round table discussion with Henk Bekedam, Marion Koopmans, Wim van der Poel and Emely de Vet. 9 March 2021 from 16.00 to 17.00, online via www.wur.nl/dies

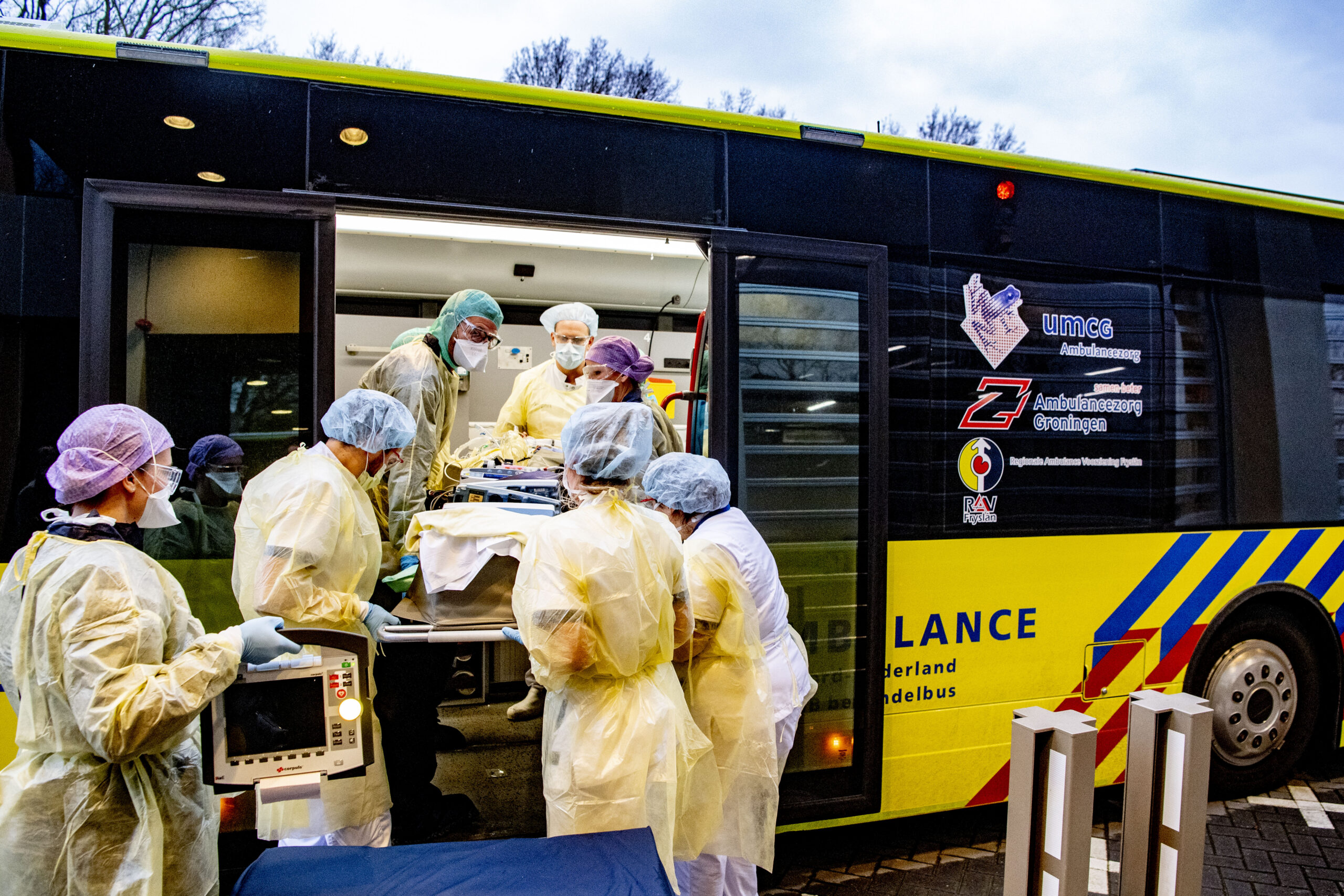 ‘Market forces have made our healthcare system very efficient, but have stripped it of the buffer with extra beds and staff that you need to cope with the initial impact of a pandemic.’ Photo ANP/ Robin Utrecht
‘Market forces have made our healthcare system very efficient, but have stripped it of the buffer with extra beds and staff that you need to cope with the initial impact of a pandemic.’ Photo ANP/ Robin Utrecht