Hanneke Moonen, a surgeon trainee at Gelderse Vallei Hospital and a PhD candidate at WUR, is studying the energy consumption of these patients both during and after their ICU stay with an eye to suitable nutritional advice. ‘Energy consumption is very variable among individuals but also in one and the same person at different moments of the day.‘
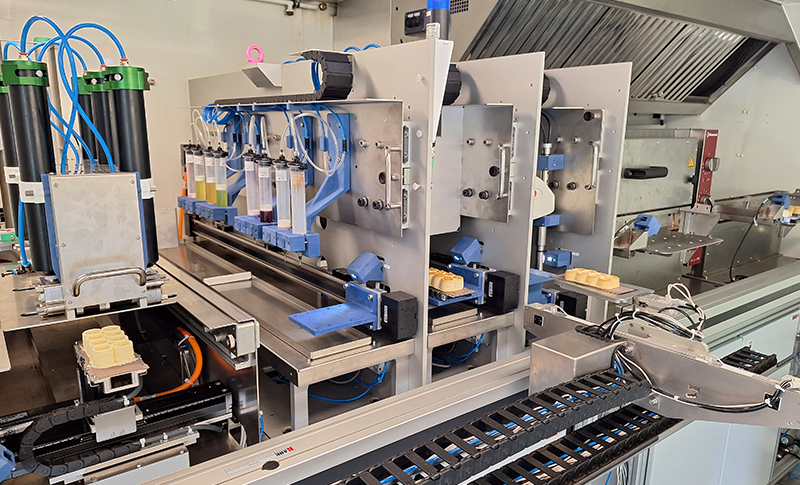
Energy consumption can be accurately determined on the basis of the ratio of oxygen and carbon dioxide in the air that someone inhales and exhales; this also applies to ICU patients. Moonen: ‘During the day the energy consumption of ICU patients is nearly stable; they spend all day being sick. That makes it easier to estimate their daily energy consumption based on a brief measurement. We can easily collect those data if patients are on a ventilator: we attach the measuring instrument to the ventilator tube. But as soon as the ventilator tube is removed, our measurements stop. At least, that’s how it always used to be.’
‘For a few years now there has fortunately been an instrument that you can connect to both the ventilator tube and a sort of astronaut helmet.’ That helmet (see photo) creates an airtight system that enables us to also accurately measure the composition of the air being inhaled and exhaled by patients without a ventilator tube. ‘Consequently, we can follow the patients’ energy consumption for a longer time.’

Difficult target group
Following these patients for a long period of time proved difficult. ‘Firstly, many patients can’t or don’t want to participate,’ Moonen explained. They themselves don’t want to or – in the case of patients with diminished consciousness – their families prefer not to. ‘And some patients who are willing to participate might undergo a treatment that makes wearing the helmet uncomfortable or that makes the results less reliable. Moreover, ICU patients are very vulnerable. Some of the patients die of their illness or because of complications. Then our measurements also stop, of course.’
However, Moonen and her colleagues were able to collect sufficient data. They followed 56 patients from the moment that they were admitted to the ICU to the moment they were dismissed from hospital or died; they collected data for 23 of these patients after they had been transferred from the ICU to the nursing ward. The results of this ‘RECOVER-Energy’ study were published last month.
Discovering patterns
Using these data the researchers tried to discover a pattern for the entire ICU population. ‘You can’t just compare the energy consumption data of individuals. A person with a large body naturally needs more energy than someone with a small body. This can be corrected for with the BMI (the body mass index, ed.), for example, but we also know that the physical composition is important because muscle tissue has a different energy need than body fat.’
With the collected data on body size and body composition, the researchers calculated a relative measure for energy consumption at rest, which enabled them to compare the data among patients.
Malnutrition
‘But we still didn’t know how this related to someone’s normal, ‘healthy’ energy consumption.’ So Moonen also looked at two different and frequently used formulas to estimate daily energy consumption in addition to the collected data. The comparison between the energy consumption at the ICU and the formulas for normal consumption showed that, after a few days, the formulas revealed an underestimation of the energy needed: ‘It’s good to realise that, if we calculate the energy needs of patients based on the standard formulas, we might be underfeeding them in as little as four days.’
Not much will change for the patients at Gelderse Vallei Hospital. ‘We already measure the energy consumption of our patients every three days. Their nutritional schedule is adjusted to this. But these results confirm that our approach is good.’

 Foto Unsplash/Marcelo Leal
Foto Unsplash/Marcelo Leal